Protocol Detail

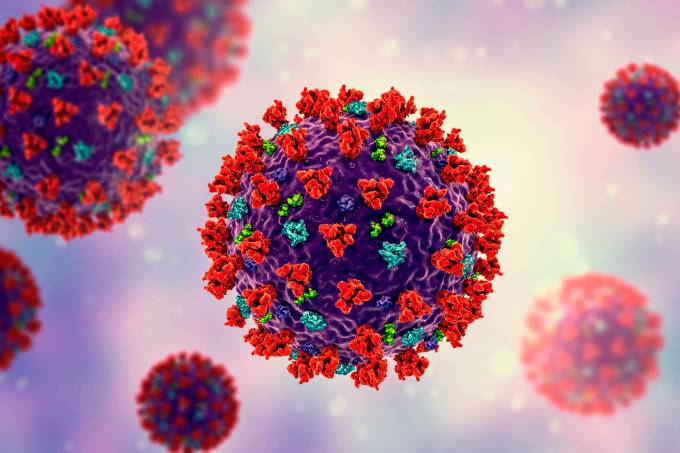
COVID 19
COVID 19 is a disease caused by the most recently discovered coronavirus which is a large family of corona viruses causing illnesses. In humans it causes Respiratory infections for example Severe Acute Respiratory Disease (SARs) PRESENTATION Fever 77-98% Cough 46-82% Myalgia/Fatigue 11-52% Shortness of breath 3-31% Incubation period 14 days, most people develop symptoms between 5-6ays from exposure Stage1 (Early infection). Stage 2. Stage 3(Hyperinflation phase) Viral response---------------------------Pulmonary Phase----------------------Host Response *Anyone presenting with flu like symptoms should be assumed to be a COVID 19 case until proven otherwise*
Diagnosis
Screening tool
Antigen test
PCR test
CXR
CT scan Chest
Bloods- FBC, CRP, IDH, U&Es.
Persistently raised inflammatory markers CRP, serum Ferritin, LDH are poor prognostic markers. Very high d-dimer- possible pulmonary embolism.
Management
Triaging
- Perform hand hygiene frequently with an alcohol based hand sanitizer (60-80% alcohol content) or wash hands with soap and running water.
- Social distancing of at least 1 meter from each other (3 feet apart) so that if one coughs/sneezes, there is less likelihood of inhaling the droplets that may have the droplets
- Early recognition of suspected COVID 19 cases, screen at arrival in hospital, isolate them in a separate room while awaiting testing. Refer appropriately
- Patients with mild symptoms should be sent home for self-quarantine for at least 14-21days
- The following patients should be considered at high risk of dying if they have COVID symptoms and should be considered for admission
- Patients with chronic diseases, for example Diabetes Mellitus, chronic lung disease, HIV Infection
- Patients older than 60
- Pregnant women
Management
- Vital observations: Patient with the vital observations below should be admitted
Temperature >= 38 degrees Celsius
Respirations above 24bpm
Pulse-rate above 120bpm
Oxygen saturation of below 90%
*Make sure to exclude other causes of fever and respiratory distress e.g. malaria, pulmonary embolism and PCP*
- Administer oxygen according to condition of patient, if in respiratory distress: Give oxygen using non rebreather mask (delivers 10 to 15litres/minute) oxygen administered per nasal prongs (delivers 5-6 L/m). If saturation remain low, use dual Oxygen therapy using both nasal prongs and non rebreather mask. If patient is not responding to dual therapy, give oxygen via high flow nasal cannula which delivers around 60-8-L/min.
- Glucometer check stat and then 4 hourly. Give insulin per sliding scale if it goes above 11.1mmols/L(The cytokine storm response which happens in COVID patients or the steroid administration both warrants glucometer checks)
- Avoid treatment with intravenous fluids unless there is obvious dehydration or septic shock (aggressive iv fluids worsen oxygenation)
- Antibiotics to curb infection. Ceftriaxone 2g IV stat then 1g 12 hourly. Azithromycin 500mg per oral on day 1 then 250mg daily x4/7
(For children give Ceftriaxone 50-80mg/kg plus Azithromycin 10mg/kg).
- Paracetamol 1gram 8 hourly per oral as an antipyretic
- For patients on oxygen, administer dexamethasone 6mg IV once daily x10/7 or until discharge (whichever comes first). Prednisolone 40mg per oral once daily.
- Coagulation common in patients with COVID 19, administer an anti-coagulant, heparin 5000 IU subcutaneously 12houly (prophylaxis) or clexane 40mg subcutaneously once daily
- Collect blood for FBC, U & E, LFT, CRP, IDH
- CXR
- Continuous monitoring of patient providing individualized care
- Discharge patient based on clinical improvement









